Top 3 Things to Look for When Auditing a Medical Manufacturer
Medical device OEMs rely on the competence and compliance of their contract manufacturers (CMs) to continuously deliver high-quality parts and products on demand. By outsourcing the production of their products, these OEMs trust those CMs with patient lives and a critical piece of the OEM’s business.
To mitigate the risks inherent in outsourcing, OEMs must audit their CMs. In the high-stakes and highly regulated world of medical devices, verification—not trust—is what’s necessary.But what exactly should OEMs verify when they audit their medical manufacturing partners? Among the numerous details covered by regulatory and ISO audits, there are a few key items that need to be included in every audit of a medical manufacturer.
Training RecordsWithout adequate training, even the most accurate and advanced inspection equipment on the market will produce wrong answers. Likewise, even the most detailed assembly work instructions assume some level of assembly skill and knowledge about how to use the necessary tools. That skill and knowledge is transferred, refreshed, and improved by training.
To ensure that the training required to produce your product is occurring, OEMs need to pay close attention to training records. During an audit, the manufacturer’s internal training records should answer “Yes” to the following questions:
Does training and re-training happen as often as it should be? If there’s a training requirement for a task or subject that is constantly evolving, there should be recurring training. How frequently it occurs depends on the specific content of training, but the manufacturer’s personnel training records and their training requirements as recorded in their internal policies should match. That documentation should also match current best practices. For example, an employee may need to receive training in basic machine shop safety only once, but more focused safety training may have to occur every time a new piece of equipment is introduced into the shop. That new machine may have unique safety features (like a light curtain) or safety hazards (e.g. laser light) which operators need to be aware of.
Are workers only performing tasks they’ve been trained on? If a new procedure or a new revision of an existing one requires training, only workers who have been trained on it should be able to sign off on the device history record (DHR) as having performed it. An audit shouldn’t uncover someone performing a new assembly or inspection procedure before they were trained on it.
When revisions change on work instructions or drawings, are all the necessary people trained? Depending on the nature of the change, regulatory requirements, and the CM quality management system (QMS) training may not be necessary for anyone. But of course, what is documented and what is done should match.Does the Whole Company Take Quality Seriously?
Thorough audits shouldn’t stop at just examining paperwork. OEMs should feel free to ask staff on the shop floor about basic quality system knowledge. They should know what their company’s quality policy is, where to find the standard operating procedures (SOPs) relevant to their jobs, and where to find the current released version of part and assembly drawings, if applicable to their job duties.
Finally, look for any processes that rely on tribal knowledge instead of a well-documented SOP. If you happen to be near a technician performing rework, ask to see the repair or assembly documentation that details the re-assembly steps or part replacement procedure. Random spot checks like these are used by FDA auditors and you should use them too.
Checking the CheckersA third area you should focus attention on is the calibration records of any test and inspection equipment used for quality control testing. It’s good practice to re-calibrate every piece of equipment every year, but in some cases, a more frequent schedule is needed. Any out of calibration equipment should be removed from the work area and set aside until serviced. Also, the certified accuracy and precision of each piece of equipment must meet or exceed the requirements of the measurements or other test results (like “go/no go” tests that use feeler gauges).
By auditing your medical contract manufacturer, you have an opportunity to verify their processes meet your standards and a chance to spot and help correct problems before the FDA does. Keeping your CM in compliance with your quality system requirements reduces your risk of adverse regulatory actions, decreases chances of supply chain disruption due to supplier noncompliance, and most importantly helps keep the patients who rely on your medical products safe.
As an FDA-registered and ISO 13485 certified medical contract manufacturer, we know firsthand the effort and diligence required to maintain a company-wide culture of quality, a culture that’s revealed in audit after audit. That’s why our OEM customers trust us with their customers, patients, and business. If you’re looking for a trustworthy medical manufacturer, give us a call.
Topics:
Related Articles
-
Oct 08, 2025
Medical Device Cleanroom Manufacturing: Plastic Injection Molding
Read MoreWhy Cleanroom Manufacturing Matters for Medical Devices
Medical devices are subject to strict...
-
Mar 17, 2025
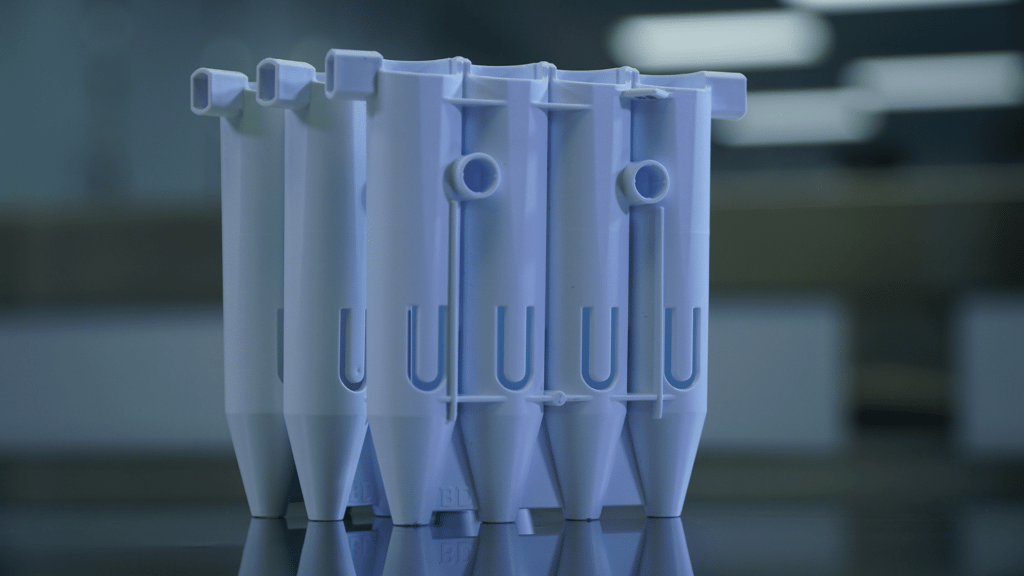
Labware & Diagnostic Injection Mold Building and Molding
Read MoreMedical device molding requires much higher levels of precision injection molding and tolerance...
-
Jan 10, 2025
Benefits of a Plastic Medical Device Manufacturer
Read MoreReusable and single-use plastic medical devices are held to high standards of sanitation, texture,...
